Polycystic ovary syndrome, often referred to as PCOS is a health condition[1] that primarily affects women of reproductive age. However, it can occur at any age after puberty and does not disappear after menopause.
PCOS occurs when androgen levels are excessive.[2] Defining polycystic ovary syndrome involves considering ovarian dysfunction in the absence of any other identifiable disease process. It’s also necessary to consider the hormonal and metabolic profile of the woman.
Historical research[3] defines PCOS only as hyperandrogenism, an Androgen Excess Society guideline statement. This definition, as we have seen, has evolved over time.
Unfortunately, untreated PCOS can lead to other health problems, such as obesity, cardiovascular disease, endometrial cancer, dyslipidemia, or diabetes. Therefore, it’s important to be aware of this condition. Below, learn about some of the top PCOS statistics, which will hopefully raise awareness.
Key PCOS Facts
- Among women, 83.0%[4] know some or less about PCOS. In men, 66.3%[4] know some or less about the condition.
- Just over half, 52.6%,[5] believe PCOS is a lifestyle disease.
- Across the globe, an estimated 5-15%[6] of women have PCOS.
- Estimates from the U.S. show that about 5.2%[7] of the population has PCOS.
- PCOS is responsible for 70%[8] of cases of anovulatory infertility.
PCOS Statistics
Self-Assessed Awareness About PCOS
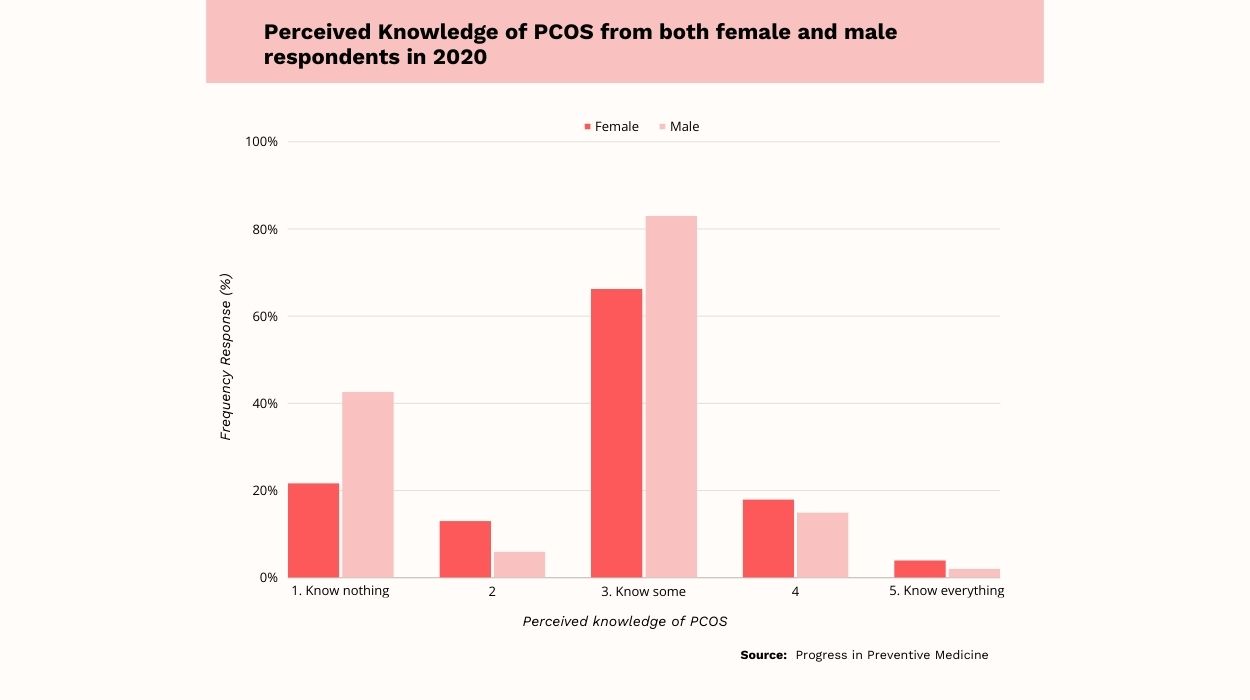
- The majority of both men and women know some or less about PCOS. More specifically, 83.0%[4] of men and 66.3%[4] of women know some or less about this condition.
- Among men, 42.6%[4] know nothing about PCOS, compared to 21.7%[4] of women.
- Just 4%[4] of women and 2.1%[4] of men report knowing everything about PCOS.
Based on the data above, most people don’t have much knowledge about PCOS. Even among women, two-thirds[4] know just some or less about PCOS. Over one-fifth[4] of women say they know nothing about PCOS.
Over eight out of 10 men[4] state they know some or less about PCOS, and over two-fifths[4] report knowing nothing. It is extremely uncommon for either men or women to know everything there is to know about PCOS.
The Population’s Knowledge About The Causes Of PCOS

- In a study assessing knowledge of PCOS, 52.6%[5] of people said they believed it was a lifestyle disease.
- An additional 10.5%[5] said they felt PCOS is due to genetic factors.
- Just 4.9%[5] of people said PCOS was a result of factors in the environment.
- 15.8%[5] believed PCOS was controlled by medications and a good lifestyle.
- Finally, 16.1%[5] of people surveyed had no idea what caused PCOS.
Over half of people believe that PCOS is a lifestyle disease. Furthermore, just over one out of 10[5] believe that genetics are responsible for polycystic ovary syndrome. Slightly more believe that it is controlled by medication and a good lifestyle.
Interestingly, nearly one-fifth[5] of people did not know what causes PCOS. This suggests there is a need for more education about women with PCOS.
PCOS Statistics For Race/Ethnicity
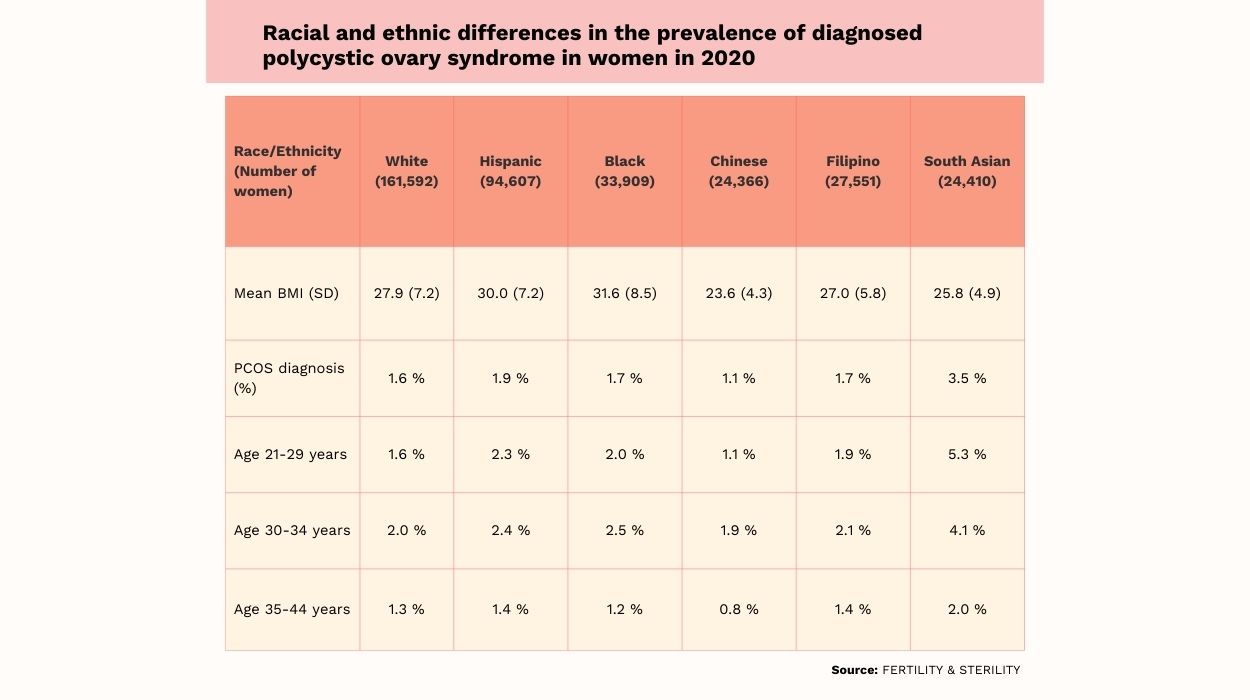
- The highest rates of PCOS are in South Asian women, for whom the prevalence is 3.5%.[9] This is followed by Hispanic women, who have a PCOS prevalence of 1.9%.[9]
- The lowest rates of PCOS are in Chinese women, for whom the prevalence is 1.1%.[9]
- Rates for White, Black, and Filipino women are all similar, at 1.6%,[9] 1.7%,[9] and 1.7%,[9] respectively.
- In South Asian women aged 21-29, the prevalence of polycystic ovary syndrome is 5.3%.[9] This category of women has the highest PCOS prevalence.
- In Chinese women aged 35-44, the prevalence of PCOS is 0.8%.[9] This category of women has the lowest prevalence.
There is variation in the prevalence of polycystic ovary syndrome by race/ethnicity and age. The highest prevalence[9] across race/ethnicity is in South Asian women, and the lowest is in Chinese women. Rates are comparable[9] among Hispanic, Black, White, and Filipino women.
Women aged 21-29 have the highest prevalence[9] of PCOS across race/ethnicity. Women aged 35-44 have the lowest prevalence[9] of PCOS.
PCOS Prevalence By Country
PCOS rates can vary by country. So, when asking how many women have PCOS, it’s important to look at where they live.
As of 2017, Educador had the highest PCOS rate, at 242.54[6] per 100,000 in the population.
Other countries in the top five list for assessing community prevalence of PCOS per 100,000 people included:
Countries with the lowest PCOS prevalence included Argentina, with 53.75[6] per 100,000 in the population. The next lowest were Uruguay, at 53.26[6] per 100,000, and Chile, at 50.69[6] per 100,000.
Prevalence Of Polycystic Ovary Syndrome In U.S. Vs. Other Countries
The data above do not mention the U.S., so it’s helpful to look at raw prevalence data for this country. According to a recent study of women in the U.S., 5.2%[7] had a PCOS diagnosis. This is four to five times the rate seen in the United Kingdom.
According to Dr. Swapna Chekuri,[10] Gynecologist, Infertility Specialist, Obstetrician, IVF, “PCOS is one of the most common hormonal disorders affecting women of reproductive age, with an estimated prevalence of 6-12%. Dr. Chekuri further states, “Evidence suggests that PCOS rates may be rising, possibly due to factors such as changes in lifestyle, environment, and genetics.”
PCOS And Fertility Statistics
PCOS is associated with infertility because hormonal imbalances can stop[1] a woman from ovulating. This doesn’t mean that a woman with PCOS cannot get pregnant. There are fertility treatments that increase the chance of pregnancy in women with polycystic ovaries.
PCOS pregnancy statistics demonstrate that pregnancy is possible with PCOS. In one study, 21.14%[11] of women without previous ovulation induction cycles became pregnant with intrauterine insemination. The women in this study were diagnosed with PCOS.
In PCOS patients, the percentage chance of getting pregnant was 23.64%[11] in those who had three or more failed attempts with ovulation induction. Fertility treatments like this are often necessary for women with PCOS. Polycystic ovarian syndrome is responsible for 70%[8] of cases of anovulatory infertility.
Statistics Of Complications Among Patients With PCOS
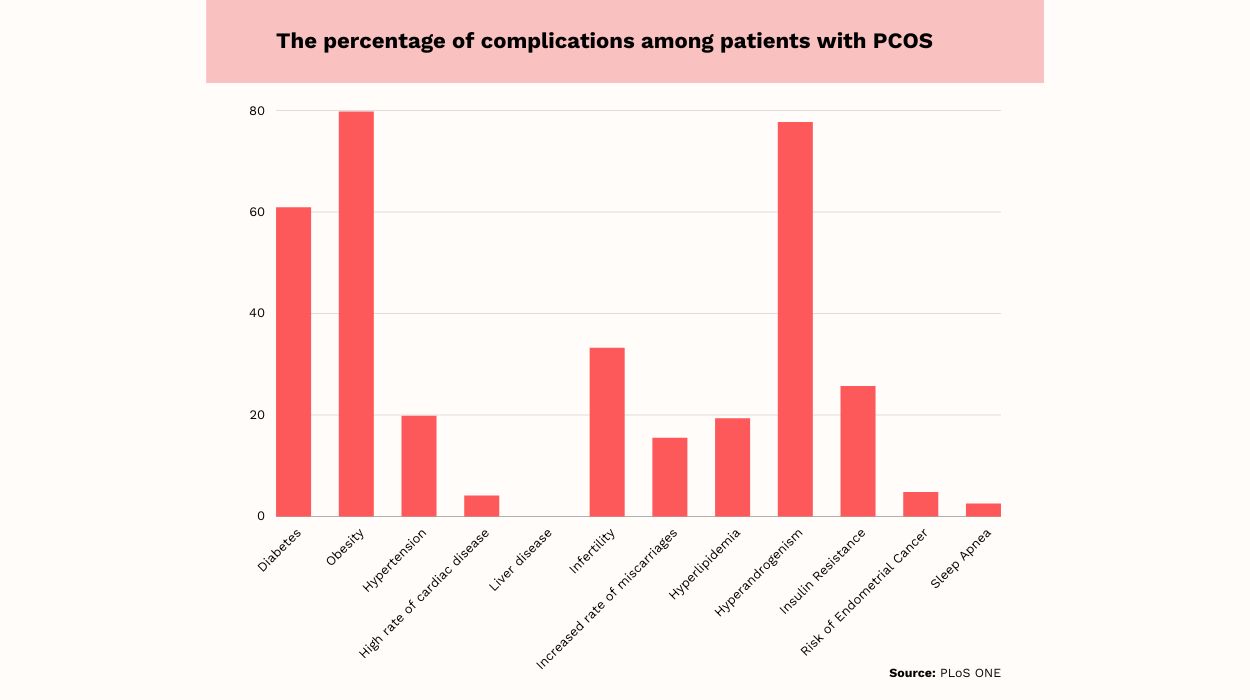
- The most common complication, affecting 80%[12] of patients with PCOS, is obesity.
- The second most common problem, hyperandrogenism, affects 77.7%[12] of those with PCOS. This refers to[13] the development of excess amounts of male hormones, primarily testosterone, in women. It causes symptoms like acne, which affects 67.3%[12] of those with PCOS.
- Diabetes is common in PCOS, as it affects 60.9%[12] of women with untreated PCOS.
- Irregular menstrual cycles affect 71.8%[12] of women with PCOS.
- Infertility is present in 33.2% of those with PCOS.
- While less common than other health problems in PCOS, 2.5%[12] of women experience sleep apnea; 19.8%[12] have hypertension, and 15.5%[12] have experienced miscarriages.
Women with PCOS are at risk of a number of health problems, especially if PCOS is untreated. A majority[12] of women with PCOS are obese, and 60.9%[12] of those with untreated PCOS are obese. High cholesterol and high blood pressure both affect about one-fifth[12] of women with untreated PCOS.
Other common problems in PCOS include irregular periods, infertility, glucose intolerance, and hyperandrogenism. Given the high prevalence of health problems, it is not surprising that 85%[12] of women with PCOS report low quality of life.
PCOS Facts To Know
Some additional interesting facts about PCOS include:
- Women with PCOS are more likely to experience depression and anxiety. In women with PCOS, 37%[14] have depression, compared to 14.2%[14] of those without PCOS. Additionally, 42%[14] of women with PCOS experience anxiety symptoms, compared to 8.5%[14] of those without PCOS.
- PCOS can start young, and it’s associated with type 2 diabetes. Research with girls diagnosed with type 2 diabetes before age 18 shows that 19.58%[15] have PCOS
- As of 2020, the healthcare costs associated with PCOS were estimated at $8 billion.[16] These costs are from diagnosis, as well as pregnancy-related expenses and the higher risk of chronic health conditions with PCOS.
- Between 1990 and 2019, the incidence of PCOS grew by 54%[17] globally. Incidence refers to new cases within a given time period.
- Globally, the incidence of PCOS is highest[17] among those aged 15-19, followed by the 10-14 age group.
How Many Women Have PCOS?
In the United States, an estimated 5.2%[7] of women have PCOS. Global data suggest that 5-15%[6] of women internationally have PCOS.
These percentages are estimates, and there can be variation based on race/ethnicity. For example, 3.5%[9] of South Asian women have PCOS, compared to 0.8%[9] of Chinese women.
Remember that when prevalence data is collected, researchers rely on data from a sample. Different samples may yield differing prevalence rates, so it can be difficult to determine the exact prevalence of PCOS.
Why Is PCOS So Common?
Global data show that the prevalence and incidence of PCOS are increasing[18] in all locations. There are several reasons that PCOS is becoming so common. These include:[18]
- Increases in sedentary behavior.
- Excessive calorie intake and obesity.
- Smoking.
- Unhealthy dietary patterns.
Lifestyle factors play a role in PCOS because these factors can lead to insulin resistance.[19] For example, being overweight from a lack of physical activity and an unhealthy diet contributes to insulin resistance. This is important because insulin resistance is linked to PCOS.
Since sedentary lifestyles and poor diet are becoming more common, insulin resistance, and thus PCOS, are also becoming more prevalent. Similarly, obesity is becoming more common, which has led to increases[20] in PCOS.
Causes Of PCOS And Risk Factors
PCOS develops when women have excess levels of hormones called androgens.[19] Insulin resistance also plays a role[19] in the development of PCOS. Weight gain and genetics can contribute to insulin resistance and therefore are also contributing factors[19] to PCOS.
Beyond insulin resistance and high androgen levels, common risk factors for polycystic ovary syndrome include:[21]
- Family history/genetic factors.
- Obesity (although most studies suggest the risk is modest).
- Having epilepsy.
- Type 1, Type 2 and gestational diabetes.
- Prenatal factors, including being born with a high birth weight to an overweight mother.
- Early puberty.
- Childhood obesity syndromes and metabolic syndrome.
Symptoms Of PCOS
PCOS symptoms include:[22]
- An irregular menstrual cycle, which can include heavy, long periods or unpredictable, absent periods.
- Presence of acne or oily skin.
- Excessive amounts of hair on the face or other body areas.
- Thinning of scalp hair or male pattern baldness.
- Weight gain, especially in the stomach.
How Is PCOS Diagnosed?
There are three diagnostic criteria for PCOS. A doctor will diagnose the condition in women who meet at least two criteria. These criteria include:[19]
- Lack of ovulation, leading to irregular periods or no periods.
- Elevated levels of male hormones called androgens, which can cause excess face and body hair, acne, and thinning hair on the scalp.
- The presence of cysts on the ovaries.
Treatments
Having PCOS increases[21] the risk of type 2 diabetes, high cholesterol, and hypertension. Given these facts, it’s important to treat PCOS and make lifestyle changes to manage the condition.
PCOS treatment typically includes[1] a combination of medication and lifestyle interventions. Treatment depends upon a woman’s unique situation and whether she’d like to become pregnant.
Lifestyle Interventions For PCOS
Lifestyle interventions, including a healthy diet and daily exercise, are recommended[1] to help with weight loss. Losing weight lowers blood sugar, reduces insulin resistance, and can make the menstrual cycle more regular. Weight loss can also help with fertility.
Women with PCOS benefit from losing weight if they would like to become pregnant. An anti-inflammatory diet low in added sugars with a low glycemic index can help lose weight and improve fertility. The Mediterranean Diet, which is high in fiber, micronutrients,, antioxidants, and monounsaturated fats, is sometimes recommended.[23]
Proinflammatory foods should be limited, emphasizing getting enough fiber, limiting total carbohydrate intake, and losing 5%-10% of body weight. Complex carbohydrates should be low-glycemic. Fats should contain optimum levels of omega-3 fatty acids, and saturated and hydrogenated fats should be restricted.
According to Dr. Himali Maniar Patel,[10] Gynecologist, MBBS, D.G.O., “While there is no known cure for PCOS, there are steps that can be taken to reverse the condition and alleviate symptoms.” He says, “One of the most effective methods is improving insulin sensitivity through lifestyle changes such as a balanced diet and regular exercise.”
Medications For PCOS
Sometimes, PCOS is treated with medications. Hormonal birth control, which could include pills, patches, shots, intrauterine devices, and vaginal rings, can be helpful.[1]
Birth control pills can regulate the menstrual cycle and reduce the risk of endometrial cancer. Birth control can also help eliminate excess hair and improve acne.
There are also anti-androgen medications[1] which block the effects of male hormones. The FDA has not approved these medications for treating PCOS, but doctors may use them. Finally, metformin, a medication used in the treatment of type 2 diabetes, can improve[1] PCOS symptoms. While not approved by the FDA for PCOS, metformin can lower blood sugar, insulin, and androgen levels. If you take metformin, make sure you take adequate supplemental vitamin D and vitamin B12.
Fertility Treatments For PCOS
Beyond weight loss, there are medical treatments[1] to help with fertility. Some doctors may prescribe medications like Clomid to promote ovulation. In vitro fertilization and surgery are also options.
Conclusion
Polycystic ovarian syndrome is a common health condition affecting 5-15%[6] of women across the globe. It causes irregular periods, infertility, and a higher risk of various health problems like diabetes and high blood pressure.
Since women with polycystic ovary syndrome are at increased risk of various health problems, treatment and lifestyle changes are important. In many cases, diet and exercise can lead to weight loss, which improves health for overweight women with PCOS.
Frequently Asked Questions
PCOS is a result of[19] insulin resistance and high levels of hormones called androgens. High androgens can stop the body from ovulating.
While PCOS can develop in a woman’s twenties or thirties, it typically begins right after a girl’s first period. This can be as young as age 10.[17] However, most women don’t realize they have PCOS until struggling to get pregnant.
Lifestyle changes, including diet and exercise, can lead to weight loss and improve PCOS symptoms. Diet and exercise can improve[24] insulin resistance, metabolic health, and reproductive functioning.
Lifestyle changes can increase the chances of becoming pregnant with PCOS. Exercise, limiting sedentary time, and weight loss can improve[23] fertility. A low-sugar, high-fiber, low-glycemic, anti-inflammatory diet is recommended.[23]
 Evidence Based
Evidence Based